Introduction:
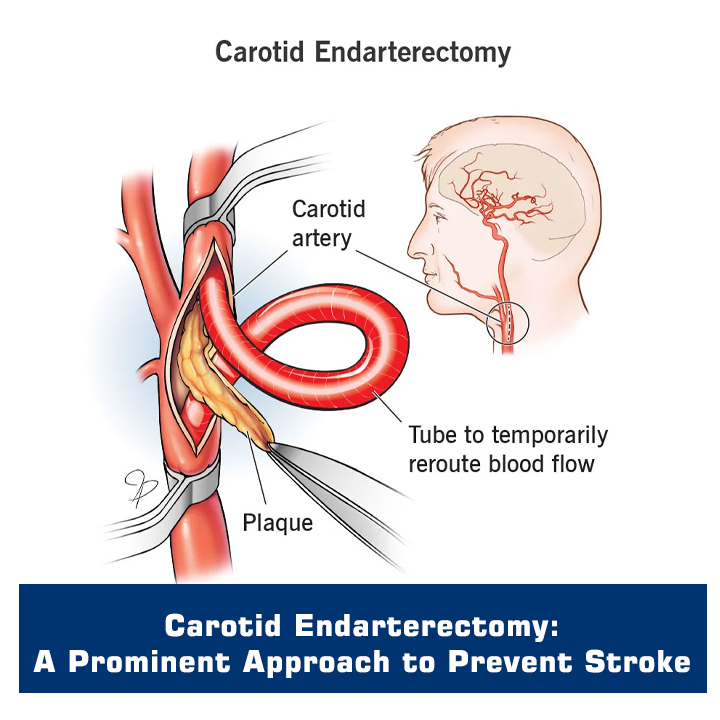
Carotid endarterectomy (CEA) is a surgical procedure aimed at treating carotid artery stenosis, a condition characterized by the narrowing of the carotid arteries that supply blood to the brain. By removing the buildup of plaque in these arteries, CEA helps prevent further strokes and improve long-term outcomes. This article provides a comprehensive guide to CEA in a question-and-answer format, covering indications for surgery, preoperative preparation, intraoperative techniques, and postoperative care.
Primary goal of carotid endarterectomy
The primary goal of carotid endarterectomy is to prevent strokes by removing the plaque buildup in the carotid arteries. By restoring proper blood flow to the brain, CEA reduces the risk of future strokes and improves overall patient outcomes.
Indications for carotid endarterectomy
Carotid endarterectomy is indicated for patients with significant carotid artery stenosis (>70% narrowing) and a recent stroke or transient ischemic attack (TIA) related to that specific artery. Additionally, patients without symptoms but with severe stenosis (>80%) may also benefit from CEA based on individual assessment.
Patients Preparation for Carotid Endarterectomy
Preoperative preparation for carotid endarterectomy involves a thorough evaluation, which includes medical history review, physical examination, and imaging studies (such as carotid ultrasound, CT angiography, or magnetic resonance angiography). Medication management, particularly blood thinners, may be adjusted before surgery. It is essential to inform the surgical team about any allergies, medical conditions, or medications.
Role of Intraoperative Neuromonitoring during Carotid Endarterectomy
Intraoperative neuromonitoring is crucial during carotid endarterectomy to assess the integrity of the brain's blood supply and neurological function. Techniques such as electroencephalography (EEG), transracial Doppler ultrasound, or somatosensory evoked potentials (SSEPs) are used to monitor the brain's electrical activity and blood flow during the surgery. This monitoring helps ensure the safety of critical neurological structures.
Procedure Performed, and What Role does the Microscope Play
Carotid endarterectomy is typically performed under general anesthesia. An incision is made along the front of the neck, and the carotid artery is exposed. The plaque is carefully removed from the artery, and the vessel is repaired with stitches or a patch. A surgical microscope is commonly used during the procedure to provide a magnified view, improving precision and minimizing the risk of damage to surrounding structures.
Carotid Endarterectomy differ from Carotid Stenting
Carotid endarterectomy and carotid stenting are two different approaches to treat carotid artery stenosis. CEA involves the surgical removal of plaque, while carotid stenting involves the placement of a stent to keep the artery open. The choice between the two procedures depends on various factors, including the patient's overall health, anatomy, and surgeon's expertise.
Postoperative Care and Long-term Outcomes
After carotid endarterectomy, patients are closely monitored in the postoperative intensive care unit (ICU) for a short period. Vital signs, neurological status, and incision site are regularly assessed. Blood thinners or antiplatelet medications may be prescribed to prevent clotting. Long-term outcomes of carotid endarterectomy are generally favorable, with a reduced risk of recurrent stroke and improved overall prognosis.
Conclusion:
Carotid endarterectomy is a vital surgical procedure for the treatment of carotid artery stenosis, aimed at preventing strokes and improving long-term outcomes. Indications for CEA include significant stenosis, recent stroke or TIA, and individual assessments. Preoperative preparation, intraoperative neuromonitoring, and the use of a microscope contribute to the safety and precision of the procedure. Distinct from carotid stenting, CEA involves the surgical removal of plaque. Postoperative care involves monitoring in the ICU, medication management, and follow-up evaluations. With careful patient selection and appropriate surgical intervention, carotid endarterectomy has shown to be effective in reducing the risk of recurrent stroke and improving long-term outcomes for patients.